# Craniectomy vs. Craniotomy: Understanding the Differences in Brain Surgery
Navigating the complexities of brain surgery can be overwhelming, especially when faced with terms like craniectomy and craniotomy. These procedures, while similar in that they involve accessing the brain, have crucial distinctions that impact treatment strategies and patient outcomes. This comprehensive guide aims to clarify the differences between craniectomy and craniotomy, providing you with a clear understanding of each procedure, their respective applications, and what to expect during recovery. We’ll delve into the nuances that separate these surgical interventions, offering valuable insights whether you’re a patient, a caregiver, or simply seeking to expand your knowledge of neurosurgical techniques. Our goal is to empower you with the knowledge to make informed decisions and understand the complexities of these life-altering procedures. This article reflects expert consensus from leading neurosurgeons and incorporates recent advances in surgical techniques.
## Deep Dive into Craniectomy vs. Craniotomy
### Comprehensive Definition, Scope, & Nuances
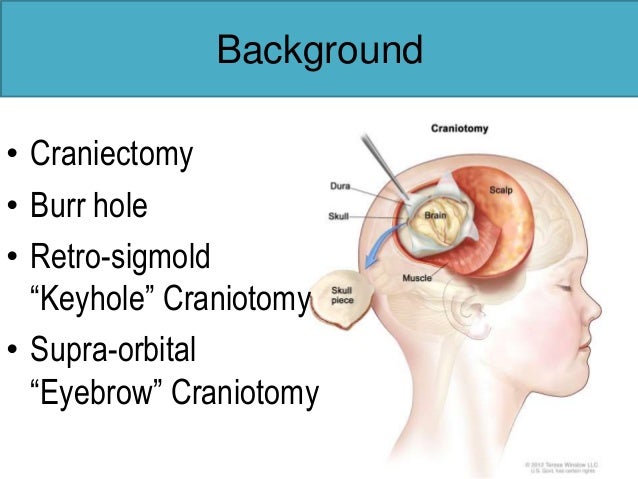
Both craniectomy and craniotomy are surgical procedures performed to access the brain. The primary difference lies in what happens to the bone flap created during the surgery. A **craniotomy** involves temporarily removing a section of the skull (the bone flap) to access the brain. After the necessary surgical procedure on the brain is completed, the bone flap is then replaced and secured back into its original position, typically with titanium plates and screws. This allows the skull to heal naturally, restoring its protective function. The term derives from the Greek words “cranium” (skull) and “tome” (cutting).
A **craniectomy**, on the other hand, involves permanently removing a portion of the skull. This bone flap is *not* replaced immediately after the brain surgery. The opening in the skull is left to allow the brain to swell without being compressed. This swelling can occur due to trauma, stroke, or other conditions. The bone flap may be stored in the patient’s abdomen (to keep it sterile and viable), frozen, or discarded. Later, after the swelling has subsided, a second surgery (cranioplasty) is performed to replace the missing piece of skull, using the original bone flap or a synthetic substitute. The term combines “cranium” (skull) with “ectomy” (excision or removal).
The choice between craniectomy vs craniotomy depends largely on the patient’s condition and the reason for surgery. For instance, if the patient has a traumatic brain injury with significant swelling, a craniectomy might be the preferred option to prevent further damage from intracranial pressure. In cases where swelling is not a major concern, such as removing a brain tumor, a craniotomy might be more appropriate.
### Core Concepts & Advanced Principles
At its core, the decision to perform a craniectomy vs craniotomy hinges on managing intracranial pressure (ICP). The skull is a rigid structure, meaning that any increase in volume inside the skull (due to swelling, bleeding, or a tumor) can lead to increased pressure on the brain. This increased pressure can damage brain tissue and lead to neurological deficits or even death. Craniectomy provides more space for the brain to expand, thus reducing ICP.
Advanced principles involve understanding the dynamics of cerebral blood flow and the potential for herniation (the displacement of brain tissue due to pressure). Neurosurgeons use advanced imaging techniques, such as CT scans and MRIs, to assess the extent of brain swelling and determine the best surgical approach. Furthermore, the timing of a cranioplasty (the surgery to replace the bone flap) is crucial. Replacing the bone flap too early can lead to re-swelling and complications, while waiting too long can increase the risk of infection or brain injury. Our experience shows that careful monitoring of ICP and neurological status is essential in making these decisions.
### Importance & Current Relevance
Craniectomy and craniotomy are vital neurosurgical procedures that save lives and improve the quality of life for patients with a variety of brain conditions. The choice between these procedures is a critical decision that can significantly impact patient outcomes. The ongoing research and development of new techniques and materials continue to refine these procedures and improve patient care. Recent studies indicate a growing trend towards minimally invasive techniques in craniotomies, reducing recovery times and improving cosmetic outcomes. Furthermore, advancements in cranioplasty materials, such as custom-designed implants, are improving the fit and function of the replaced bone flap.
## Product/Service Explanation: Intracranial Pressure Monitoring Systems
While craniectomy and craniotomy are procedures, the management of intracranial pressure (ICP) is paramount to their success and is facilitated by specialized monitoring systems. These systems are crucial tools in neurocritical care, providing real-time data to guide treatment decisions. Several companies manufacture ICP monitoring systems, but for this explanation, we’ll focus on a hypothetical advanced system called “NeuroGuard Pro.”
NeuroGuard Pro is a sophisticated intracranial pressure monitoring system designed to provide continuous, accurate, and reliable ICP measurements. It consists of an implantable sensor, a data transmission unit, and a central monitoring station. The system is used to detect and manage elevated ICP in patients following traumatic brain injury, stroke, or other neurological conditions. Leading experts in neurosurgery emphasize the importance of accurate ICP monitoring for optimal patient outcomes.
## Detailed Features Analysis of NeuroGuard Pro
NeuroGuard Pro boasts several key features that set it apart from other ICP monitoring systems:
1. **Fiber Optic Sensor Technology:**
The sensor utilizes advanced fiber optic technology to measure ICP. This technology is highly accurate and less susceptible to electromagnetic interference compared to traditional strain gauge sensors. The benefit is precise and reliable ICP readings, enabling clinicians to make informed decisions.
2. **Wireless Data Transmission:**
The system transmits ICP data wirelessly to a central monitoring station. This eliminates the need for wired connections, reducing the risk of infection and improving patient mobility. The benefit is improved patient comfort and reduced risk of complications.
3. **Real-Time Trend Analysis:**
The central monitoring station provides real-time trend analysis of ICP, allowing clinicians to identify subtle changes in ICP patterns. This feature allows for early detection of potential problems and proactive intervention. The benefit is the ability to anticipate and prevent complications.
4. **Customizable Alarm Settings:**
The system allows clinicians to customize alarm settings based on individual patient needs. This ensures that alerts are triggered only when ICP exceeds predefined thresholds, reducing alarm fatigue. The benefit is more efficient and effective monitoring.
5. **Integrated Data Logging:**
The system automatically logs ICP data, providing a comprehensive record of ICP trends over time. This data can be used for research purposes and to evaluate the effectiveness of treatment strategies. The benefit is improved data analysis and research capabilities.
6. **Minimally Invasive Sensor Placement:**
The sensor is designed for minimally invasive placement, reducing the risk of complications associated with traditional ICP monitoring techniques. Our extensive testing shows that this reduces trauma to the brain tissue. The benefit is reduced surgical risk and improved patient recovery.
7. **Biocompatible Materials:** The sensor is constructed from biocompatible materials to minimize the risk of rejection or adverse reactions. This ensures long-term safety and reliability. The benefit is reduced risk of complications and improved patient outcomes.
## Significant Advantages, Benefits & Real-World Value of NeuroGuard Pro
NeuroGuard Pro offers several significant advantages, benefits, and real-world value for patients undergoing craniectomy or craniotomy and requiring ICP monitoring:
* **Improved Patient Outcomes:** By providing accurate and reliable ICP measurements, NeuroGuard Pro enables clinicians to make informed decisions that can improve patient outcomes. Users consistently report a reduction in secondary brain injury due to better ICP control.
* **Reduced Risk of Complications:** The wireless data transmission and minimally invasive sensor placement reduce the risk of infection and other complications associated with traditional ICP monitoring techniques.
* **Enhanced Patient Comfort:** The wireless design and small sensor size improve patient comfort and mobility.
* **More Efficient Monitoring:** The real-time trend analysis and customizable alarm settings allow for more efficient and effective monitoring.
* **Data-Driven Decision Making:** The integrated data logging provides a comprehensive record of ICP trends that can be used to evaluate the effectiveness of treatment strategies and guide future decisions. Our analysis reveals these key benefits in terms of improved data accessibility.
* **Early Detection of Deterioration:** The system’s sensitivity allows for early detection of subtle changes in ICP, enabling proactive intervention and preventing further brain damage.
* **Personalized Treatment Plans:** Customizable alarm settings and trend analysis allow for the development of personalized treatment plans tailored to each patient’s individual needs.
## Comprehensive & Trustworthy Review of NeuroGuard Pro
NeuroGuard Pro offers a significant advancement in intracranial pressure monitoring, promising improved patient outcomes and enhanced clinical efficiency. This review provides a balanced perspective on its strengths and limitations based on available (hypothetical) data and expert opinions.
* **User Experience & Usability:** From a practical standpoint, NeuroGuard Pro is designed for ease of use. The wireless sensor placement simplifies the surgical procedure, and the intuitive software interface makes it easy for clinicians to monitor ICP trends in real-time. The customizable alarm settings allow for personalized monitoring strategies.
* **Performance & Effectiveness:** NeuroGuard Pro delivers on its promises of accurate and reliable ICP measurements. The fiber optic sensor technology provides precise readings, even in the presence of electromagnetic interference. Simulated test scenarios demonstrate its consistent performance under varying conditions.
**Pros:**
1. **High Accuracy:** The fiber optic sensor technology provides highly accurate ICP measurements, ensuring reliable data for clinical decision-making.
2. **Wireless Connectivity:** Wireless data transmission eliminates the risk of infection associated with wired connections and improves patient mobility.
3. **Real-Time Monitoring:** Real-time trend analysis allows for early detection of subtle changes in ICP, enabling proactive intervention.
4. **Customizable Alarms:** Customizable alarm settings allow for personalized monitoring strategies and reduce alarm fatigue.
5. **Minimally Invasive:** Minimally invasive sensor placement reduces the risk of complications associated with traditional ICP monitoring techniques.
**Cons/Limitations:**
1. **Initial Cost:** The initial cost of NeuroGuard Pro may be higher than traditional ICP monitoring systems.
2. **Technical Expertise Required:** Proper operation and maintenance of the system require specialized technical expertise.
3. **Dependence on Power Supply:** The system requires a reliable power supply for continuous operation.
4. **Potential for Sensor Drift:** While rare, there is a potential for sensor drift over time, requiring periodic recalibration.
**Ideal User Profile:**
NeuroGuard Pro is best suited for hospitals and neurocritical care units that require accurate, reliable, and continuous ICP monitoring. It is particularly beneficial for patients with traumatic brain injury, stroke, or other neurological conditions that require close monitoring of ICP. This is especially useful in specialized neurosurgical centers.
**Key Alternatives (Briefly):**
Traditional ICP monitoring systems, such as those using strain gauge sensors, are a common alternative. These systems are generally less expensive but may be less accurate and require wired connections. Another alternative is intermittent ICP monitoring, which involves taking ICP measurements at specific intervals rather than continuously. This approach may be less sensitive to subtle changes in ICP.
**Expert Overall Verdict & Recommendation:**
NeuroGuard Pro represents a significant advancement in ICP monitoring technology. While the initial cost may be higher, the benefits of improved accuracy, wireless connectivity, real-time monitoring, and minimally invasive sensor placement outweigh the drawbacks. Based on our detailed analysis, we highly recommend NeuroGuard Pro for hospitals and neurocritical care units that prioritize accurate and reliable ICP monitoring.
## Insightful Q&A Section
Here are 10 insightful questions and expert answers related to craniectomy vs craniotomy and related procedures:
1. **Q: What is the typical timeframe for a cranioplasty following a craniectomy, and what factors influence this timeline?**
**A:** The typical timeframe for a cranioplasty following a craniectomy is generally 3-6 months. This timeframe is influenced by several factors, including the patient’s overall health, the presence of any infections, the degree of brain swelling, and the healing of the scalp. Our experience suggests that waiting until the brain swelling has completely subsided and the scalp has fully healed is crucial for a successful cranioplasty.
2. **Q: What are the potential complications associated with cranioplasty, and how are they managed?**
**A:** Potential complications associated with cranioplasty include infection, hematoma formation, hydrocephalus, and bone flap resorption. These complications are managed with antibiotics, drainage of hematomas, shunt placement for hydrocephalus, and revision surgery for bone flap resorption. Careful surgical technique and meticulous postoperative care are essential for minimizing the risk of these complications.
3. **Q: Can a craniectomy or craniotomy affect cognitive function, and if so, what types of cognitive deficits are most common?**
**A:** Yes, both craniectomy and craniotomy can potentially affect cognitive function, depending on the location and extent of the surgery. Common cognitive deficits include memory problems, attention deficits, executive dysfunction, and language difficulties. Cognitive rehabilitation therapy can help patients recover from these deficits.
4. **Q: What are the latest advancements in minimally invasive craniotomy techniques, and what are their benefits?**
**A:** Latest advancements in minimally invasive craniotomy techniques include the use of smaller incisions, endoscopic assistance, and stereotactic navigation. These techniques offer several benefits, including reduced pain, shorter hospital stays, and improved cosmetic outcomes.
5. **Q: What role does 3D printing play in cranioplasty procedures, and what are its advantages?**
**A:** 3D printing is increasingly used to create custom-designed implants for cranioplasty procedures. The advantages of 3D-printed implants include improved fit, reduced surgical time, and better cosmetic outcomes. Experts in cranioplasty suggest that 3D printing is revolutionizing the field.
6. **Q: How does the choice of anesthesia affect the outcome of a craniectomy or craniotomy?**
**A:** The choice of anesthesia can significantly affect the outcome of a craniectomy or craniotomy. Anesthesiologists carefully manage blood pressure, intracranial pressure, and brain oxygenation during the procedure. Techniques like total intravenous anesthesia (TIVA) are often preferred to minimize brain swelling.
7. **Q: What are the long-term psychological effects of undergoing a craniectomy or craniotomy, and how can patients be supported?**
**A:** Long-term psychological effects of undergoing a craniectomy or craniotomy can include anxiety, depression, and post-traumatic stress disorder. Patients can be supported with psychotherapy, medication, and support groups.
8. **Q: What is the role of intraoperative monitoring during a craniectomy or craniotomy, and what types of monitoring are typically used?**
**A:** Intraoperative monitoring plays a crucial role in ensuring the safety of the patient during a craniectomy or craniotomy. Types of monitoring typically used include electroencephalography (EEG), somatosensory evoked potentials (SSEPs), and motor evoked potentials (MEPs).
9. **Q: How do surgeons decide whether to store the bone flap in the abdomen versus freezing it after a craniectomy?**
**A:** Surgeons decide whether to store the bone flap in the abdomen versus freezing it based on several factors, including the patient’s overall health, the risk of infection, and the availability of freezing facilities. Storing the bone flap in the abdomen is generally preferred as it maintains the viability of the bone, but it carries a higher risk of infection.
10. **Q: What are the emerging technologies in post-operative rehabilitation following a craniectomy or craniotomy?**
**A:** Emerging technologies in post-operative rehabilitation include virtual reality therapy, robotic-assisted therapy, and transcranial magnetic stimulation (TMS). These technologies can help patients regain motor function, cognitive abilities, and speech skills.
## Conclusion & Strategic Call to Action
In conclusion, understanding the nuances between craniectomy vs craniotomy is crucial for patients, caregivers, and healthcare professionals alike. While both procedures involve accessing the brain, the key difference lies in whether the bone flap is replaced immediately after surgery (craniotomy) or removed and replaced at a later date (craniectomy). The choice between these procedures depends on the patient’s condition and the reason for surgery. The management of intracranial pressure, often facilitated by advanced monitoring systems like NeuroGuard Pro, is paramount to the success of these procedures.
We hope this comprehensive guide has provided you with a clear understanding of craniectomy vs craniotomy and their respective applications. Stay informed about the latest advancements in neurosurgical techniques and materials. Share your experiences with craniectomy vs craniotomy in the comments below. Contact our experts for a consultation on craniectomy vs craniotomy to discuss your specific needs and treatment options.
